Intermittent Fasting and Autophagy: The Science
Understanding Autophagy
Autophagy, a fascinating cellular process, is essentially the body's built-in recycling system. It's a complex mechanism where cells break down and recycle damaged or unnecessary components, including proteins, organelles, and even entire cellular structures. This process is vital for maintaining cellular health and preventing the accumulation of cellular debris, which can lead to various diseases. Think of it as a cellular spring cleaning, ensuring the cells are functioning optimally.
This natural process is critical for eliminating damaged proteins and organelles, preventing the buildup of harmful substances, and maintaining cellular homeostasis. It's a fundamental aspect of cellular health, directly impacting overall well-being and resilience.
Autophagy and Cellular Damage
Damaged proteins and organelles, if not properly removed, can accumulate within the cell, leading to various cellular stress responses. This accumulation can cause significant damage, impacting cellular function and potentially contributing to the development of diseases. Autophagy plays a crucial role in mitigating this damage, ensuring the cells can effectively manage and eliminate these harmful components.
The Role of Nutrients in Autophagy
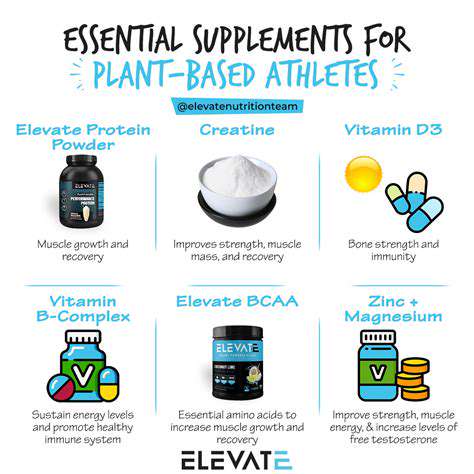
Nutrients play a significant role in stimulating or inhibiting autophagy. Certain nutrients, like amino acids, can trigger autophagy by providing the building blocks necessary for the process. Conversely, excessive caloric intake can sometimes hinder autophagy, potentially leading to adverse health effects. Understanding the interplay between nutrition and autophagy is crucial for optimizing cellular health.
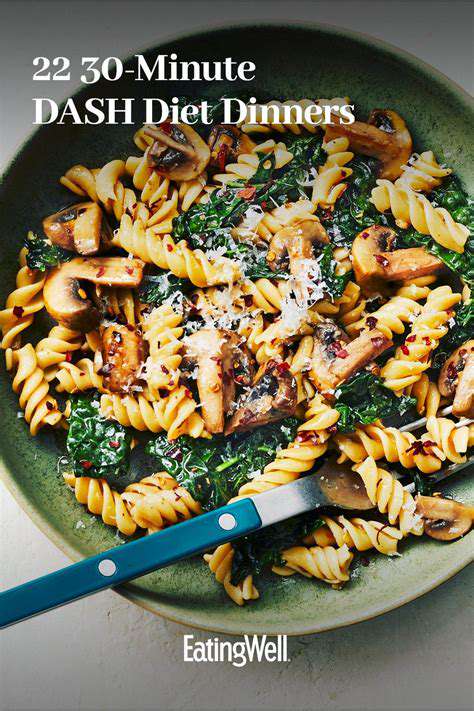
Caloric restriction, for example, is often associated with increased autophagy. This suggests that a well-balanced nutritional approach, potentially including intermittent fasting, can play a key role in supporting this vital cellular process.
Intermittent Fasting and Autophagy Induction
Intermittent fasting (IF) has emerged as a potential tool for inducing autophagy. By strategically restricting food intake, IF can create a cellular environment conducive to autophagy. During periods of fasting, the body may prioritize the breakdown and recycling of cellular components, potentially leading to increased autophagy activity. This is a promising avenue for research and exploring the potential health benefits of IF.
Autophagy and Disease Prevention
Autophagy's role in preventing and mitigating diseases is a significant area of ongoing research. Studies suggest that increased autophagy activity can protect cells from damage caused by various stressors, potentially reducing the risk of neurodegenerative diseases, cardiovascular diseases, and certain cancers. The protective effect of autophagy on cellular health is a compelling reason to explore its potential benefits in disease prevention.
Future Directions in Autophagy Research
Further research into the mechanisms of autophagy and its interaction with other cellular processes is crucial for unlocking its full therapeutic potential. Scientists are actively investigating how autophagy can be modulated to treat various diseases. Understanding the intricate pathways involved in autophagy regulation will be essential for developing targeted therapies and interventions. This is a dynamic field with exciting potential for future advancements in medical science.
The ongoing research into autophagy promises to offer exciting insights into its role in promoting health and preventing disease. Understanding the mechanisms involved and the specific ways to modulate autophagy will be crucial for developing future therapeutic approaches.
How Intermittent Fasting Potentially Enhances Autophagy

Potential Benefits of Intermittent Fasting
Intermittent fasting (IF) is a dietary approach that cycles between periods of eating and voluntary fasting. This approach has garnered significant attention for its potential health benefits beyond weight management. Studies suggest that IF may play a role in improving insulin sensitivity, reducing inflammation, and potentially impacting cellular repair processes. Understanding the mechanisms behind these effects can offer insight into the potential benefits of incorporating IF into a healthy lifestyle.
One compelling area of research is the potential impact of IF on metabolic health. Numerous studies indicate that IF can lead to improvements in blood sugar control, cholesterol levels, and blood pressure. These improvements are attributed to various mechanisms, including enhanced insulin sensitivity and reduced oxidative stress. It's important to note that the effectiveness of IF can vary depending on individual factors, such as age, activity levels, and overall health.
Metabolic Effects and Insulin Sensitivity
A key aspect of IF's potential is its impact on insulin sensitivity. When you fast, your body shifts its energy source from glucose to fat, which can lead to improved insulin sensitivity over time. This enhanced sensitivity means that your body can better utilize insulin to regulate blood sugar levels, which is crucial for preventing type 2 diabetes and managing existing conditions.
Further research is needed to fully understand the long-term effects of intermittent fasting on metabolic health. However, the current evidence suggests that IF can significantly improve metabolic markers, potentially reducing the risk of chronic diseases. Consistent dietary changes, including IF, should be discussed with a healthcare professional to determine if they are suitable for your individual needs.
Cellular Repair and Autophagy
One intriguing aspect of intermittent fasting is its potential role in cellular repair and the process of autophagy. Autophagy is a cellular recycling process where damaged or dysfunctional cellular components are broken down and recycled, promoting cellular health and potentially reducing the risk of age-related diseases. Studies have shown a correlation between IF and increased autophagy activity, suggesting a potential link between fasting and cellular rejuvenation.
Potential Risks and Considerations
While intermittent fasting shows promise, it's important to acknowledge potential risks and considerations. Individuals with certain medical conditions, such as diabetes or eating disorders, should consult with their healthcare provider before implementing any significant dietary changes. Sudden or drastic changes in eating habits can sometimes lead to digestive issues, fatigue, or headaches in some people. Furthermore, individual responses to IF can vary considerably, and what works for one person might not be suitable for another. Careful monitoring and adjustments are often necessary to find the optimal approach to intermittent fasting.
Important Considerations and Caveats
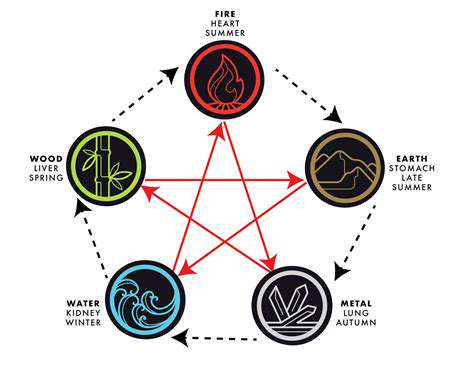
Metabolic Flexibility and Adaptability
Understanding how intermittent fasting (IF) impacts metabolic flexibility is crucial. Metabolic flexibility refers to the body's ability to switch between burning glucose and fat for energy. IF, by creating periods of reduced calorie intake, can promote this adaptability. This allows the body to utilize stored fat more efficiently, which is a key component of many health benefits associated with IF. The body learns to utilize fat as a primary fuel source, potentially leading to improved insulin sensitivity and overall metabolic health. This process is a cornerstone of the scientific understanding of how IF can positively influence health outcomes.
However, individual responses to IF can vary significantly. Some individuals may find it easier to adapt their metabolism to burning fat, while others may experience a more gradual adjustment. Factors like genetics, existing health conditions, and lifestyle choices play a role in determining how the body responds to IF protocols.
Potential Impact on Hormone Regulation
Intermittent fasting has been linked to changes in hormone levels, particularly insulin, growth hormone, and cortisol. These hormonal shifts can influence various bodily functions, including metabolism, appetite, and stress response. Understanding these hormonal effects is essential for assessing the potential impact of IF on overall health. While generally considered positive, the nuanced effects of IF on hormone regulation require careful consideration and ongoing research.
The changes in hormone levels during fasting periods can have both positive and negative consequences. It's important to monitor individual responses and consult with a healthcare professional to ensure that any hormonal adjustments are within a healthy range. This is particularly important for individuals with existing hormonal imbalances.
Individual Differences and Considerations
Not everyone responds to intermittent fasting in the same way. Individual factors like age, gender, activity level, and overall health status can significantly influence the effectiveness and safety of IF. It's important to acknowledge that what works well for one person might not be suitable for another. This is a crucial point to remember when considering adopting IF as a lifestyle choice. Understanding individual variances is paramount for safe and effective implementation.
Consulting with a healthcare professional is highly recommended before starting any new dietary regimen, including intermittent fasting. This is particularly important for individuals with pre-existing health conditions, such as diabetes, or those taking medications. A doctor can assess individual needs and tailor any dietary changes accordingly, ensuring the safety and efficacy of the approach.
Potential Gastrointestinal Effects
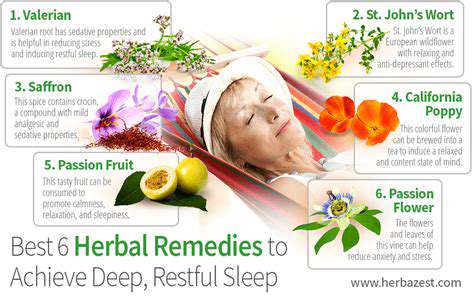
Some individuals may experience gastrointestinal (GI) side effects when starting intermittent fasting, such as hunger pangs, headaches, or digestive discomfort. These effects are often temporary and resolve as the body adapts to the new eating pattern. It is important to listen to your body and adjust the fasting schedule or duration as needed.
However, persistent or severe GI issues should be addressed by a medical professional. These issues could indicate underlying health problems or an inappropriate approach to intermittent fasting.
Safety and Long-Term Sustainability
While intermittent fasting is often considered safe for healthy individuals, it's crucial to approach it with caution and prioritize long-term sustainability. The safety and long-term implications of different IF protocols still need to be fully understood through research. Carefully monitored protocols and regular check-ins with healthcare providers are essential components of a safe IF approach.
The long-term effects and safety of IF are still being investigated. The research is ongoing, and it is important to remain aware of the evolving understanding of this approach. Sustaining the regimen over extended periods requires careful consideration and potentially requires adjustments based on individual circumstances.
Social and Practical Considerations
Social situations and practical aspects of daily life can significantly affect the ability to maintain an intermittent fasting schedule. Mealtimes with friends and family, social events, or unexpected circumstances might require adjustments to the fasting plan. Flexibility and adaptability are key to navigating these situations effectively. Careful planning and communication are important to manage these potential challenges.
Realistically assessing the challenges of incorporating IF into your current routine is vital. Finding methods to make it work within your existing lifestyle and social commitments is important. Creating a support network and exploring different IF approaches can significantly enhance the long-term success of adopting this dietary pattern.