GAPS Diet Success Stories: Inspiring Transformations

Understanding the GAPS Diet Fundamentals
The GAPS diet, short for Gut and Psychology Syndrome diet, focuses on healing the gut-brain connection, offering a unique approach to wellness by targeting digestive health. Many people struggling with chronic issues find that traditional methods don't address the root causes of their discomfort. This nutritional protocol stands out because it looks beyond symptoms to heal the digestive system at its core.
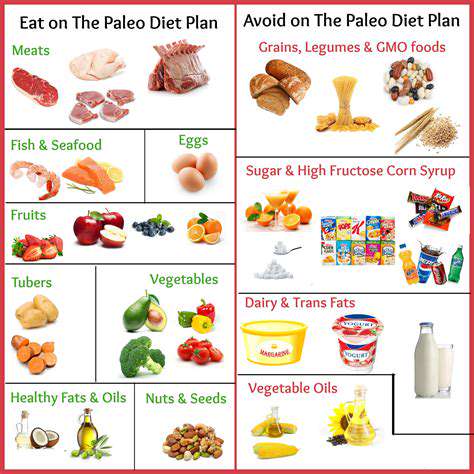
Dietary Restrictions and Guidelines
The GAPS protocol requires eliminating foods that commonly cause inflammation or digestive distress. Processed foods, refined sugars, and common allergens like gluten disappear from the plate, replaced by nutrient-dense whole foods. While the transition can feel overwhelming at first, numerous testimonials highlight how these changes lead to remarkable health transformations. The diet's phased approach helps individuals gradually adapt to their new way of eating.
Introduction of Specific Food Groups
Healing begins with simple, easily digestible foods that nourish without overwhelming a compromised system. Nutrient-rich bone broth serves as a cornerstone, providing essential minerals and collagen to repair the gut lining. As healing progresses, the diet carefully reintroduces foods to test tolerance and ensure continued progress.
Importance of Gut Microbiome
Modern science continues to reveal how profoundly gut bacteria influence overall health. A balanced microbiome doesn't just aid digestion - it supports immune function, mental health, and even influences weight management. The GAPS diet specifically targets this complex ecosystem, using food as medicine to restore microbial balance. Many followers report improvements in conditions they never associated with gut health.
Addressing Mental Health Concerns
Unexpected benefits often emerge as the gut heals, particularly in cognitive function and emotional wellbeing. The gut-brain axis explains how digestive health directly impacts neurotransmitter production and brain function. While dietary changes alone may not resolve all mental health challenges, they frequently create a foundation for more effective treatment when combined with other therapies.
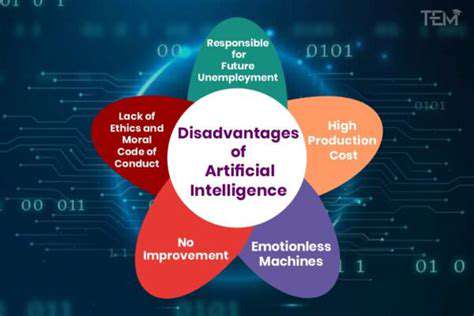
Potential Benefits and Drawbacks
Those considering the GAPS diet should weigh its potential rewards against the required commitment. While many experience reduced inflammation and improved digestion, the intensive nature of the protocol demands significant lifestyle adjustments. Transition periods can be challenging, making professional guidance invaluable for navigating the process successfully.
Long-Term Sustainability and Lifestyle Changes
True healing requires patience and persistence beyond initial dietary changes. The most successful GAPS diet followers integrate its principles into a sustainable, long-term approach to eating rather than viewing it as a temporary fix. Personalization becomes key as individuals learn which foods support their unique biology best. This adaptive approach helps maintain benefits while allowing for life's variations.
Addressing Autoimmune Conditions with GAPS
Understanding Autoimmune Diseases
Autoimmune disorders represent one of medicine's most complex challenges, where the body's defense mechanisms turn against its own tissues. These conditions manifest in countless ways, each with its own constellation of symptoms. The immune system's sophisticated network, designed for protection, becomes the source of harm in these cases. This paradox makes treatment particularly challenging.
Genetic predispositions combine with environmental triggers to create the perfect storm for autoimmune activation. Infections, stress, and dietary factors may all contribute to tipping the immune system into dysfunction. Understanding these multifaceted origins helps explain why autoimmune conditions vary so widely between individuals.
Diagnosis and Testing Procedures
Identifying autoimmune conditions involves piecing together clues from bloodwork, symptoms, and medical history. Specialized tests can detect specific antibodies that indicate particular autoimmune responses. However, the path to diagnosis often requires persistence as symptoms may evolve over time.
Physicians must consider the whole clinical picture since autoimmune markers sometimes appear before symptoms develop. This diagnostic complexity underscores the importance of working with knowledgeable healthcare providers who understand these conditions' nuances.
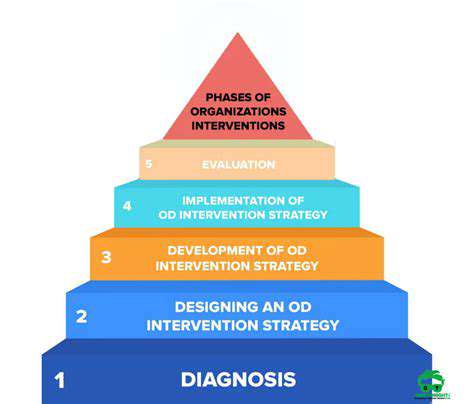
Treatment Approaches and Management Strategies
Effective autoimmune management typically combines medical interventions with lifestyle modifications. While medications help regulate immune activity, dietary changes often provide complementary support. The GAPS approach offers a nutritional strategy that may help calm excessive immune responses in some individuals.
Successful management requires active patient participation. Learning to recognize personal triggers and responses empowers individuals to become partners in their care rather than passive recipients of treatment.
Lifestyle Modifications for Improved Outcomes
Daily habits significantly influence autoimmune disease progression and symptom severity. Beyond dietary changes, stress reduction techniques and sleep hygiene play crucial roles. Many find that addressing these foundational aspects of health creates a more stable platform for other treatments to work effectively.
Emerging research continues to uncover connections between lifestyle factors and immune regulation. This growing body of evidence supports the value of comprehensive approaches that extend beyond pharmaceutical interventions.
The Role of Medical Professionals
Navigating autoimmune conditions benefits greatly from a collaborative healthcare team. Specialists in immunology work alongside nutritionists and other practitioners to create individualized plans. This team approach helps address the multiple systems affected by autoimmune processes.
Regular monitoring allows for timely adjustments to treatment strategies as conditions evolve. This dynamic approach acknowledges that autoimmune diseases rarely follow static, predictable courses.
Research and Future Directions
The field of autoimmune research continues to make exciting advances in understanding these complex conditions. Scientists are unraveling how genetic, environmental, and microbial factors interact to trigger immune dysregulation. These insights are leading to more targeted therapies with fewer side effects.
Future treatments may include personalized immunomodulation based on an individual's unique immune signature. Such advancements promise to transform autoimmune care from symptom management to potential prevention and reversal of disease processes.