Intermittent Fasting and Hormonal Balance

Insulin Sensitivity and Blood Sugar Control
Insulin, a crucial hormone for regulating blood sugar levels, is significantly impacted by IF. Intermittent fasting can improve insulin sensitivity, meaning your body utilizes insulin more effectively to move glucose from your bloodstream into your cells. This improved sensitivity can lead to better blood sugar control, a key benefit for individuals with prediabetes or type 2 diabetes and those looking to maintain healthy blood sugar levels. Fasting can also reduce the body's reliance on insulin for glucose uptake, potentially leading to a more stable metabolic profile.
The mechanisms behind this improved insulin sensitivity are complex and involve various cellular processes. Studies suggest that IF can promote the growth and function of insulin-producing cells in the pancreas, as well as increase the number of insulin receptors on cells throughout the body, allowing for better glucose uptake.
Growth Hormone Secretion
Growth hormone (GH) plays a vital role in cell repair, muscle growth, and overall body composition. Intermittent fasting is often associated with a surge in GH release, particularly during the overnight fast and in the initial phases of a fast. This surge can contribute to increased muscle mass, reduced body fat, and improved bone density.
This GH release is often observed during sleep and following a period of fasting, potentially because the body is prioritizing energy expenditure and repair during these times of reduced energy availability.
Cortisol Regulation
Cortisol, a stress hormone, plays a role in regulating metabolism, blood pressure, and immune function. While chronically high cortisol levels can be detrimental, moderate cortisol fluctuations are often part of a healthy response to stress and can also be influenced by IF. Strategic intermittent fasting can help to regulate cortisol levels, preventing excessive spikes and promoting a more balanced hormonal environment.
However, it's important to note that the impact of IF on cortisol levels can vary depending on individual factors, including stress levels and the specific fasting protocol followed. Careful monitoring and adjustment of the fasting schedule might be necessary to optimize cortisol regulation.
Thyroid Hormone Function
Thyroid hormones, including T3 and T4, are essential for regulating metabolism, energy expenditure, and numerous other bodily functions. Intermittent fasting may influence thyroid function, but the effect is not as consistently pronounced as with insulin or growth hormone. While some studies suggest a positive correlation between IF and thyroid hormone levels, more research is needed to fully understand the complex interplay.
Leptin and Ghrelin Balance
Leptin and ghrelin are hormones involved in regulating appetite and energy balance. Leptin is often associated with feelings of fullness, while ghrelin stimulates hunger. Intermittent fasting can influence the balance between these two hormones, potentially leading to improved appetite control and reduced cravings. This can contribute to better weight management and overall metabolic health. The changes in these hormones during intermittent fasting are a complex interplay and are still under active investigation.
Further research is needed to fully elucidate the precise mechanisms by which IF impacts the intricate interplay between leptin and ghrelin, and how this contributes to long-term metabolic regulation.
A digital twin, in the context of logistics, is a virtual representation of a physical process or asset. This virtual replica mirrors the real-world counterpart, capturing its characteristics, behavior, and performance. It's not just a static image, but a dynamic model that can be used to simulate various scenarios and predict potential issues. This allows businesses to gain a comprehensive understanding of their logistics operations, from warehouse management to delivery routes, and ultimately optimize their processes.
Individual Variations and Considerations

Individual Genetic Variations
Understanding the vast array of genetic variations within a population is crucial for personalized medicine. These variations, often subtle differences in DNA sequences, can significantly impact an individual's response to medications, susceptibility to diseases, and overall health trajectory. Identifying these specific variations is essential for tailoring treatments and preventative measures to maximize effectiveness and minimize adverse effects.
Environmental Influences
Beyond genetics, environmental factors play a vital role in shaping individual health outcomes. Exposure to pollutants, diet, lifestyle choices, and social determinants of health all contribute to the complex interplay that defines an individual's well-being. These environmental influences are often intertwined with genetic predispositions, creating a nuanced picture of health risks and resilience.
Lifestyle Choices
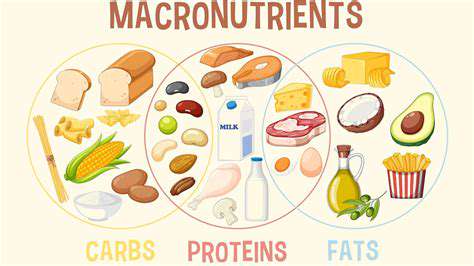
The choices we make daily, from dietary habits to exercise routines, have a profound impact on our health. A balanced diet rich in fruits, vegetables, and whole grains, combined with regular physical activity, can significantly reduce the risk of chronic diseases. Conversely, unhealthy habits can contribute to a range of health problems, highlighting the importance of proactive lifestyle choices.
Cultural Backgrounds
Cultural backgrounds often dictate dietary preferences, social norms, and access to healthcare resources. These factors can significantly influence individual health outcomes. Understanding the diverse cultural contexts is essential for developing culturally sensitive and effective health interventions. Recognizing the unique needs and perspectives of different cultures is crucial for promoting equitable health care.
Socioeconomic Status
Socioeconomic factors such as income, education, and access to resources have a profound impact on health. Individuals with lower socioeconomic status often experience disparities in access to quality healthcare, nutritious food, and safe living environments. These disparities contribute to health inequities, highlighting the urgent need for interventions that address the social determinants of health.
Psychological Factors
Mental well-being and psychological factors are integral components of overall health. Stress, anxiety, and depression can significantly impact physical health and increase the risk of various diseases. Promoting mental health through access to support systems, therapy, and stress management techniques is vital for improving individual well-being. Addressing mental health needs is essential to achieving holistic health and preventing adverse health outcomes.
Medical History and Family History
An individual's medical history, including past illnesses, surgeries, and treatments, provides valuable insights into their health status and potential risks. Family history also plays a critical role, as genetic predispositions to certain diseases can be passed down through generations. Combining these historical factors with current health data creates a comprehensive picture of an individual's health profile, allowing for more personalized and effective healthcare strategies. This combined understanding leads to more accurate risk assessments and tailored preventative measures.