TCM for Insomnia: Restoring Restful Sleep Naturally
Acupuncture and other TCM Techniques for Insomnia Relief
Acupuncture's Historical Roots
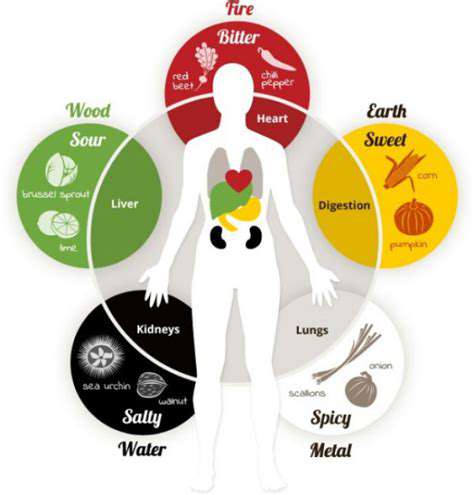
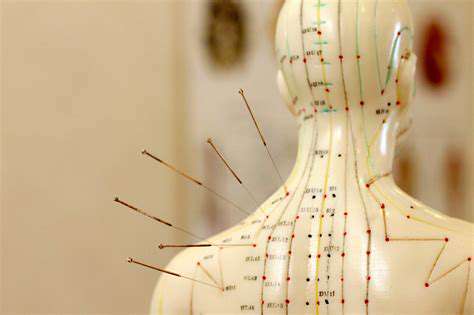
For millennia, Traditional Chinese Medicine (TCM) has relied on acupuncture as a foundational therapy. The art of strategically placing needles to restore energy flow emerged in ancient China, with practitioners meticulously refining their techniques over generations. These early healers mapped the body's Qi pathways, developing a sophisticated system that addressed both physical and energetic imbalances. Today's acupuncture sessions still echo these ancient principles.
Historical medical texts reveal acupuncture's surprising versatility, treating everything from digestive issues to emotional distress. Unlike symptom-focused Western approaches, this tradition sought to identify and correct underlying imbalances. The philosophy emphasized prevention as much as cure, viewing health as a dynamic equilibrium between body and environment.
Modern Applications of Acupuncture
Far from being obsolete, acupuncture continues gaining recognition in contemporary healthcare. Cutting-edge neuroscience research now validates what practitioners observed centuries ago - targeted needle stimulation triggers measurable physiological responses. Clinical trials demonstrate particular promise for managing chronic pain, though many patients report unexpected benefits like improved digestion and emotional resilience.
Corporate wellness programs increasingly include acupuncture sessions to combat work-related stress. The treatment's ability to induce deep relaxation makes it valuable in our high-pressure society. Unlike pharmaceutical interventions, acupuncture works with the body's natural healing mechanisms rather than overriding them.
Other TCM Techniques
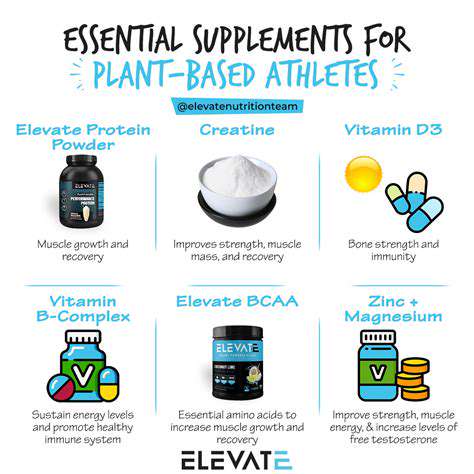
The TCM toolkit extends far beyond acupuncture needles. Custom herbal formulations represent another pillar of treatment, with combinations tailored to individual constitutional patterns. Master herbalists consider not just symptoms but also seasonal influences and emotional factors when preparing remedies.
Modern phytochemistry confirms the therapeutic compounds in many traditional herbs, though TCM's true innovation lies in their synergistic combinations. A qualified practitioner might prescribe chrysanthemum for its calming properties while adding goji berries to support adrenal function. These nuanced prescriptions reflect TCM's complex diagnostic framework.
The Holistic Approach of TCM
TCM's greatest strength may be its integrated perspective on health. Practitioners assess patients through multiple lenses - pulse diagnosis, tongue examination, and detailed questioning about lifestyle habits. This comprehensive evaluation reveals connections between seemingly unrelated symptoms that conventional medicine often misses.
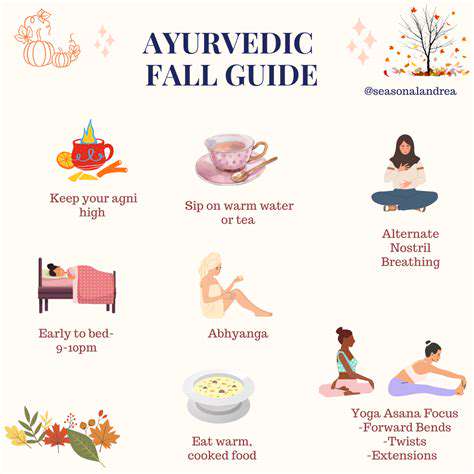
Treatment plans frequently include dietary recommendations based on energetic food properties rather than just nutritional content. For instance, a patient with dampness symptoms might reduce dairy while increasing bitter greens. Such personalized guidance exemplifies how TCM empowers patients to participate actively in their healing process.
Lifestyle Changes for Improved Sleep Quality
Dietary Adjustments for Better Sleep
What we eat profoundly influences sleep architecture. Heavy evening meals force digestion when the body should be winding down, so finishing dinner 3-4 hours before bed helps. Tart cherry juice provides natural melatonin, while magnesium-rich pumpkin seeds support muscle relaxation. Surprisingly, a small protein snack before bed can prevent blood sugar drops that disrupt sleep.
Hydration timing matters as much as quantity. Front-loading water intake earlier in the day prevents midnight bathroom trips. Herbal teas like chamomile or passionflower make excellent evening beverages, offering hydration without caffeine's stimulating effects. Remember that dietary changes require patience - it takes about three weeks for the body to adapt to new nutritional patterns.
Stress Management Techniques for Peaceful Nights
The body's stress response directly competes with sleep physiology. Simple breathing exercises can short-circuit this - try the 4-7-8 method (inhale 4 counts, hold 7, exhale 8). Many find journaling effective for downloading worries from mind to paper. The key is consistency; even five minutes daily builds resilience over time.
Creating a sensory transition ritual signals bedtime approaching. This might involve diffusing lavender oil while doing gentle neck stretches. Blue light blocking glasses worn after sunset help maintain natural melatonin production. The routine's predictability trains the nervous system to recognize sleep time, making the transition smoother.
Regular Exercise and Physical Activity for Enhanced Sleep
Movement acts as a natural sleep regulator, but timing proves crucial. Morning sunlight exposure combined with exercise helps set circadian rhythms. Yoga's dual focus on movement and breath makes it particularly sleep-friendly. Even non-traditional activities like gardening or dancing count - the goal is consistent movement you enjoy.
Post-exercise, the body undergoes repair processes that complement sleep. However, intense workouts within 3 hours of bedtime may backfire by raising core temperature. Gentle evening walks can actually promote sleep by facilitating the natural temperature drop that precedes drowsiness. Listen to your body's signals - some thrive on evening exercise while others need earlier activity.