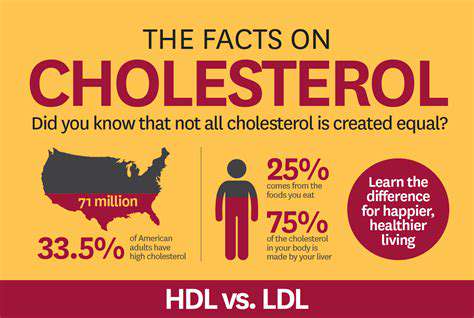
Understanding Cholesterol: Good vs. Bad Fats
Cholesterol travels through our bloodstream via specialized carriers called lipoproteins. Low-density lipoprotein (LDL) often earns the label bad cholesterol because elevated levels may lead to arterial plaque formation, raising cardiovascular risks. In contrast, high-density lipoprotein (HDL) acts as the good cholesterol by scavenging excess cholesterol from arteries and transporting it to the liver for elimination.
Factors Affecting Cholesterol Levels
Multiple elements influence cholesterol concentrations, including nutritional habits, genetic predisposition, and daily routines. Diets heavy in saturated and trans fats typically elevate LDL levels, while meals abundant in plant-based foods help maintain balance. Some individuals inherit tendencies toward higher cholesterol regardless of lifestyle. Additionally, sedentary behavior and tobacco use can negatively alter cholesterol profiles. Recognizing these interconnected factors empowers better cholesterol management.
The Role of Diet in Cholesterol Management
Food choices significantly sway cholesterol measurements. Animal products and processed items containing saturated fats often increase LDL concentrations. Conversely, soluble fiber from oats, legumes, and fruits helps reduce circulating LDL. Including beneficial fats from avocados, nuts, and olive oil supports healthier cholesterol ratios. A thoughtful, balanced approach to nutrition forms the foundation for cholesterol control.
Lifestyle Choices for Healthy Cholesterol
Daily habits profoundly impact cholesterol beyond just dietary factors. Regular physical activity boosts HDL while decreasing LDL levels. Maintaining appropriate body weight prevents cholesterol imbalances associated with excess fat. Eliminating tobacco use provides immediate benefits to cholesterol profiles and cardiovascular health overall. These lifestyle adjustments create powerful, lasting improvements in cholesterol measurements.
Cholesterol and Cardiovascular Health
Elevated LDL cholesterol poses serious risks to heart and vascular health. Arterial plaque accumulation from excessive LDL narrows blood vessels, potentially leading to life-threatening blockages. Recognizing this connection motivates proactive cholesterol monitoring and management. Understanding these mechanisms helps prevent catastrophic cardiovascular events.
Testing and Monitoring Cholesterol Levels
Regular blood tests provide crucial insights into cholesterol status. Comprehensive panels measure LDL, HDL, and total cholesterol values. Consistent medical check-ups combined with healthy living enable optimal cholesterol maintenance. Learning to interpret these results facilitates informed decisions about health strategies. Ongoing monitoring proves essential for preserving cardiovascular wellness.
The Different Types of Cholesterol: Good vs. Bad
Understanding the Basics of Cholesterol
This essential fatty substance exists throughout our bodies, contributing to cell structure and hormone production. Excessive blood cholesterol nevertheless increases cardiovascular risks. Distinguishing between cholesterol types and their health impacts forms the basis of preventive care.
Two primary cholesterol carriers exist: low-density (LDL) and high-density (HDL) lipoproteins. LDL transports cholesterol to tissues but may deposit excess in arteries, while HDL removes surplus cholesterol for disposal.
Low-Density Lipoprotein (LDL) Cholesterol
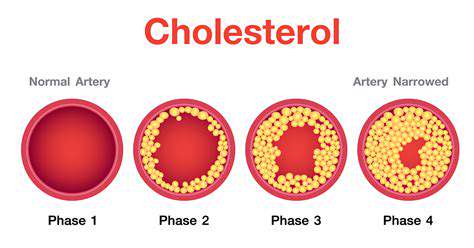
As the main cholesterol transporter, LDL poses risks when overabundant. Arterial plaque formation from accumulated LDL restricts blood flow. This progressive narrowing can culminate in heart attacks or strokes, making LDL management critical.
High-Density Lipoprotein (HDL) Cholesterol
HDL benefits cardiovascular health by clearing cholesterol from circulation. Higher HDL concentrations correlate with reduced heart disease risk as it returns cholesterol to the liver for processing. Lifestyle factors powerfully influence HDL levels.
Triglycerides
Though structurally different from cholesterol, these blood fats interact metabolically. Elevated triglycerides combined with unfavorable LDL/HDL ratios compound cardiovascular dangers. Dietary control and physical activity help regulate triglyceride levels.
Other Factors Affecting Cholesterol Levels
Multiple influences shape cholesterol profiles. Genetic predisposition interacts with modifiable factors like nutrition and activity levels. Smoking and excess weight negatively impact cholesterol balance. Comprehensive assessment of these variables enables personalized management strategies.
Managing Your Cholesterol
Effective cholesterol control combines dietary modifications, regular exercise, and weight management. Professional medical guidance ensures appropriate interventions based on individual risk factors. Proactive cholesterol monitoring facilitates timely adjustments to health strategies.
Managing Your Cholesterol: Lifestyle Choices Matter

Dietary Changes for Cholesterol Management
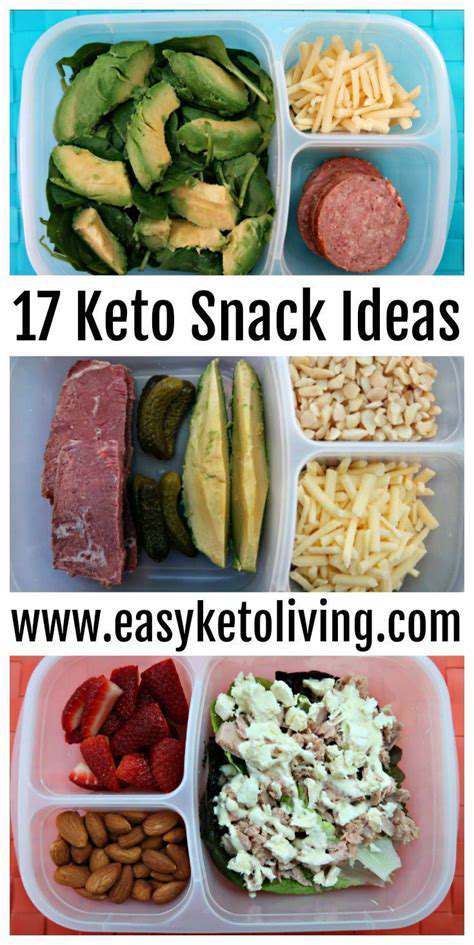
Heart-conscious eating patterns significantly influence cholesterol levels. Emphasizing whole, minimally processed foods provides optimal nutrition while reducing harmful fats. Fiber-rich plant foods actively lower LDL concentrations. Healthier fat sources like olive oil and nuts improve lipid profiles. Lean protein selections including fish and legumes support balanced cholesterol metabolism.
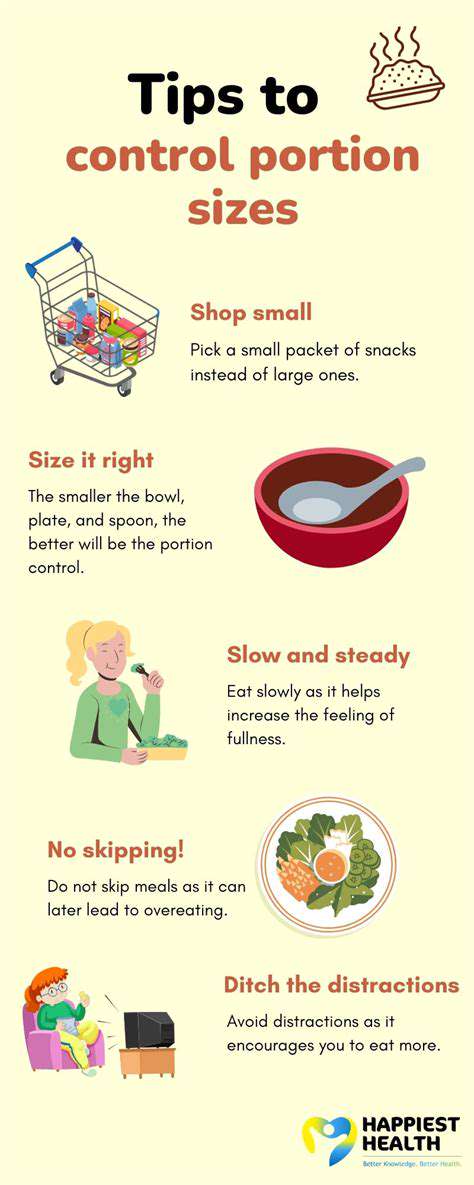
Moderating high-cholesterol foods like shellfish preserves balance. Appropriate portion control and meal frequency prevent excessive intake. Soluble fiber from specific grains and legumes impedes cholesterol absorption. Strategic dietary planning yields cumulative benefits for cholesterol regulation.
Physical Activity and Cholesterol Control
Regular movement powerfully modifies cholesterol measurements. The recommended 150 weekly minutes of moderate exercise elevates HDL while reducing LDL. Strength training complements aerobic activity by enhancing metabolic efficiency. Enjoyable physical activities promote sustained participation and lasting cholesterol improvements.
Incorporating movement into daily routines amplifies health benefits. Simple choices like stair climbing or walking breaks enhance cholesterol management. Consistent physical activity maintains cardiovascular health beyond just cholesterol effects. Professional guidance ensures appropriate exercise programming for individual needs.
Beyond Diet: Medical Interventions for High Cholesterol
Statin Therapy: A Cornerstone of Treatment
Statins represent first-line pharmaceutical options that inhibit hepatic cholesterol production. Extensive research confirms their effectiveness in cardiovascular risk reduction. Potential muscular or hepatic side effects necessitate medical supervision. Individualized dosing considers patient-specific factors for optimal outcomes.
Bile Acid Sequestrants: Binding the Excess
These agents interrupt bile acid recycling, forcing cholesterol utilization for bile synthesis. Generally well-tolerated, they may cause mild digestive discomfort. Often combined with other therapies, they require consideration of potential medication interactions.
Ezetimibe: Blocking Cholesterol Absorption
This medication specifically targets intestinal cholesterol uptake. Particularly beneficial for dietary cholesterol challenges, it frequently augments statin therapy. The dual mechanism provides comprehensive cholesterol reduction.
PCSK9 Inhibitors: Targeting a Specific Pathway
These advanced biologics disrupt PCSK9 protein function, dramatically lowering LDL levels. Reserved for severe or resistant cases, they represent cutting-edge cholesterol management. Their development illustrates ongoing pharmaceutical innovation.
Lifestyle Modifications: The Foundation of Treatment
Therapeutic interventions work best alongside healthy living practices. Nutritional improvements, physical activity, and weight control synergize with medications. These fundamental changes provide comprehensive cardiovascular protection.
Dietary Changes: Choosing the Right Foods
Strategic food selection remains crucial despite medical treatments. Reducing harmful fats while increasing beneficial nutrients optimizes therapy effectiveness. Understanding food-cholesterol relationships informs better dietary decisions.
Monitoring and Follow-up: Ongoing Care is Essential
Regular cholesterol testing tracks intervention effectiveness. Continuous medical supervision allows timely treatment adjustments. This proactive approach ensures optimal long-term cholesterol management and cardiovascular protection.