Understanding Gluten Sensitivity: Beyond Celiac Disease
What is Gluten Sensitivity?
What Causes Gluten Sensitivity?
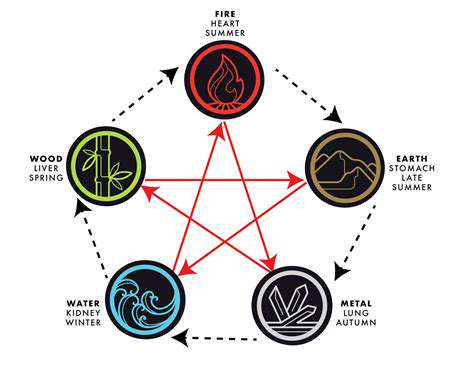
Gluten sensitivity remains a puzzling condition for both researchers and doctors. This issue arises when people experience negative reactions after consuming gluten, a protein present in wheat, barley, and rye. While science hasn't fully cracked the code behind this condition, several factors seem to contribute. Genetics play a key role, with certain individuals being more prone to developing sensitivity due to their genetic makeup. These genetic differences might cause the immune system to overreact to gluten, leading to inflammation and various uncomfortable symptoms.
Beyond genetics, environmental elements also come into play. The balance of bacteria in our gut, along with our dietary habits and lifestyle choices, might influence how our bodies respond to gluten. Researchers are particularly interested in how different forms of gluten protein interact with our digestive system. Even the way gluten-containing foods are prepared could affect how people react to them. Understanding these complex interactions remains an important area of study for scientists trying to solve the gluten sensitivity puzzle.
Symptoms and Diagnosis of Gluten Sensitivity
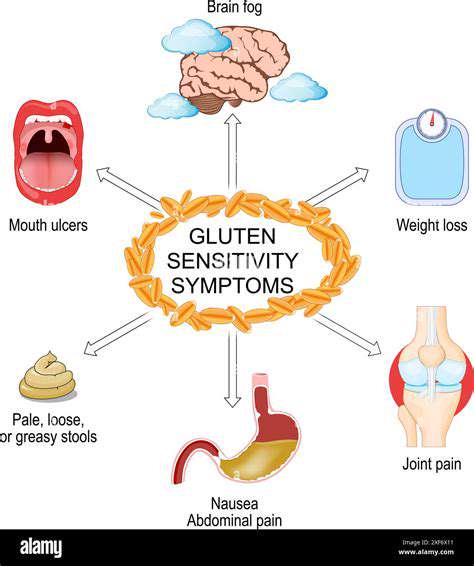
Spotting gluten sensitivity can be tricky because symptoms vary widely from person to person. Some people might experience mild stomach discomfort, while others face more serious whole-body reactions. Common digestive complaints include feeling bloated, stomach aches, and irregular bowel movements. These issues might come and go, making them harder to pin down. Interestingly, problems aren't limited to digestion - many people report tiredness, headaches, skin issues, and joint pain alongside their stomach troubles.
Diagnosing this condition requires careful detective work by medical professionals. There's no single test that can confirm gluten sensitivity, so doctors use multiple approaches. They'll start by discussing your medical history and eating habits in detail. Special blood tests can check how your immune system reacts to gluten. In some cases, doctors might use a tiny camera to look inside your digestive tract for signs of irritation. The most telling test often involves trying a gluten-free diet, then carefully reintroducing gluten to see if symptoms return.
It's absolutely crucial to work with a doctor rather than trying to self-diagnose. Healthcare providers can properly evaluate your symptoms, run the right tests, and create a personalized plan to manage your condition. Getting the right diagnosis makes all the difference in finding effective ways to feel better and avoid potential health complications.
Diagnosing Non-Celiac Gluten Sensitivity
Understanding Non-Celiac Gluten Sensitivity
Non-celiac gluten sensitivity describes people who react poorly to gluten but don't have celiac disease. Scientists are still working to understand exactly how this happens, but the immune system definitely gets involved when gluten enters the picture. The wide range of possible symptoms - from stomach issues to brain fog - makes this condition particularly hard to identify and diagnose.
This condition can affect people in very different ways, impacting everything from digestion to daily energy levels. Figuring out what specifically triggers reactions and how the body responds forms the foundation for managing symptoms effectively.
Symptoms of Non-Celiac Gluten Sensitivity
The signs of NCGS can be all over the map, often looking like other health issues, which creates real diagnostic challenges. Many people report stomach bloating, pain, diarrhea, and constant tiredness as primary complaints. Others experience headaches, trouble concentrating, skin problems, or even mood changes like anxiety.
What makes diagnosis especially difficult is how symptoms can range from mild to severe and appear at unpredictable times. Sometimes reactions don't show up immediately after eating gluten, leading to confusion about what's actually causing the problem.
Diagnosis Challenges
Identifying NCGS presents doctors with significant hurdles because no specific test exists for it. The symptoms mirror many other digestive disorders, and patients often have inconsistent reactions. This overlap makes it hard to separate NCGS from conditions like irritable bowel syndrome or food intolerances.
The Role of Dietary Restrictions
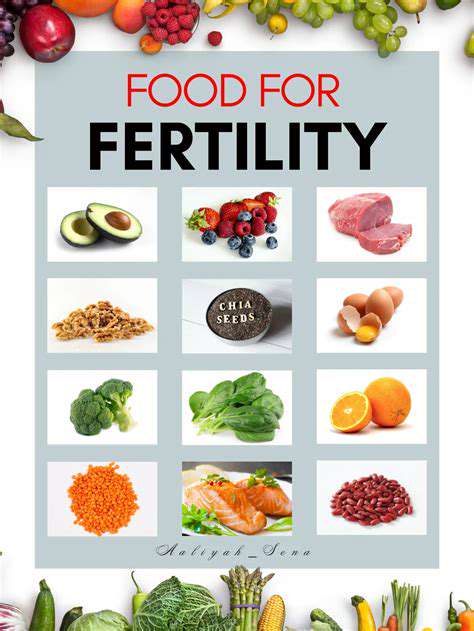
Managing NCGS often starts with cutting out gluten-containing foods, which can lead to dramatic improvements in how people feel. However, the degree of improvement varies widely - some people notice changes quickly, while others see more gradual benefits.
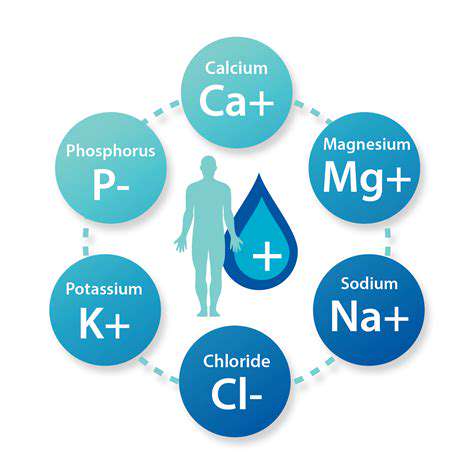
While going gluten-free helps many, it's smart to work with a nutrition professional. They can help create an eating plan that avoids gluten while ensuring you still get all necessary nutrients, as gluten-free diets can sometimes lead to nutritional gaps.
Importance of Medical Consultation
Getting professional medical advice is essential for properly identifying and managing NCGS. A doctor can thoroughly evaluate your symptoms, perform necessary tests, and rule out other possible conditions that might be causing similar issues.
Seeing a digestive specialist (gastroenterologist) is particularly valuable as they have specific expertise in these types of conditions. They can guide you through the diagnostic process and help develop an effective management strategy tailored to your needs.
Managing NCGS Effectively
Successfully living with NCGS usually involves more than just dietary changes. While avoiding gluten forms the foundation, other lifestyle factors also play important roles. Managing stress levels, drinking enough water, and maintaining overall healthy habits can all contribute to feeling better.
Getting to the root of what triggers your symptoms and understanding your body's unique responses is key for long-term management. Keeping careful notes about what you eat and how you feel afterward can reveal important patterns that help guide your treatment approach.