The History of TCM: Ancient Wisdom for Modern Health
Early Influences and Philosophies
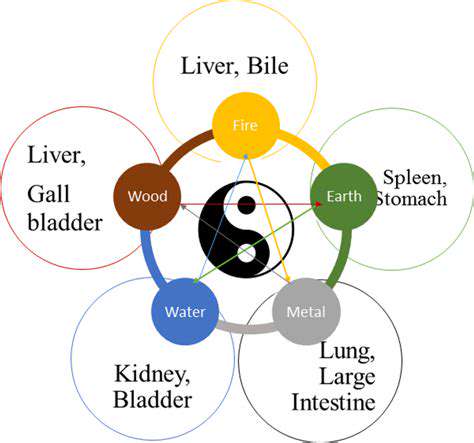
The origins of Traditional Chinese Medicine (TCM) stretch back through millennia, deeply intertwined with ancient Chinese worldviews and careful observations of nature's rhythms. For generations, scholars and healers have meticulously documented the dynamic interplay between yin and yang forces, the five elemental phases (wood, fire, earth, metal, water), and the vital life force known as Qi. This comprehensive framework views human health as inseparable from environmental harmony, distinguishing TCM from more compartmentalized medical approaches.
Foundational texts like the Huangdi Neijing (Yellow Emperor's Inner Canon) established core TCM principles that continue to guide practice today. These early medical compendiums explored bodily systems through the lens of energetic balance, where illness represented disrupted harmony rather than isolated pathology. The concept of individualized treatment emerged from this perspective, recognizing that identical symptoms might stem from different root imbalances.
The Development of Acupuncture and Moxibustion
Acupuncture represents one of TCM's most recognizable practices, employing hair-thin needles to influence Qi flow through an elaborate meridian network. Over centuries, practitioners refined this art, mapping hundreds of precise points that correspond to specific physiological and energetic functions. While modern science continues investigating its mechanisms, clinical experience demonstrates acupuncture's value particularly for pain modulation and functional disorders where conventional options prove limited.
Moxibustion complements acupuncture by applying smoldering mugwort near key points to warm and invigorate Qi circulation. This technique exemplifies TCM's innovative use of thermal therapy, where carefully controlled heat application produces therapeutic effects distinct from simple temperature changes. The selection of moxibustion points follows the same diagnostic logic as needle placement, demonstrating TCM's systematic approach to treatment.
Herbal Medicine's Vital Role
With over 3,000 documented medicinal substances, TCM's pharmacopeia represents one of the world's most sophisticated herbal systems. Practitioners combine botanicals in complex formulas where ingredients interact synergistically, with lead herbs targeting primary symptoms while supporting herbs enhance effects and minimize side reactions. The art of herbal prescription lies in customizing classic formulas to each patient's unique pattern, adjusting composition and dosage based on continuous reassessment.
The Evolution of Diagnosis Techniques
TCM assessment methods form a sophisticated observational science developed through centuries of clinical refinement. Pulse diagnosis evaluates twenty-eight distinct qualities at three positions on each wrist, revealing systemic information far beyond simple heart rate. Tongue examination analyzes color, coating, moisture, and morphology as external markers of internal conditions. This diagnostic approach excels at detecting functional disturbances before they manifest as structural pathology, offering valuable opportunities for preventive intervention.
TCM's Impact on Modern Healthcare
Contemporary medicine increasingly recognizes TCM's contributions, particularly in managing chronic conditions where purely biochemical models prove inadequate. Areas like psycho-emotional disorders, functional gastrointestinal issues, and stress-related syndromes respond well to TCM's regulatory approaches. The World Health Organization's inclusion of TCM diagnostic categories in ICD-11 signifies growing international acceptance, though integrating these ancient practices with modern standards requires thoughtful adaptation.
Integrating TCM into Modern Practices
Successful integration demands mutual understanding between conventional and traditional practitioners. Hospital-based TCM departments in China demonstrate effective collaboration models, where Western diagnostics identify structural abnormalities while TCM addresses functional aspects. Standardized training programs and quality-controlled herbal products help bridge the gap, though cultural differences in medical philosophy remain the most significant challenge to seamless integration.
The Future of TCM
Emerging technologies like AI-assisted pattern recognition and metabolomic analysis of herbal effects are revolutionizing TCM research. Contemporary practitioners increasingly combine ancient diagnostic methods with modern imaging and lab tests, creating comprehensive patient profiles. The next frontier involves developing bilingual clinical language that accurately conveys TCM concepts to Western-trained colleagues while preserving their philosophical depth.
From Emperors' Courts to Modern Clinics: The Evolution of TCM Practice
From Imperial Grandeur to Everyday Elegance
The transition of TCM from exclusive imperial courts to community clinics mirrors broader societal transformations. Ancient medical knowledge once reserved for royalty became democratized through generations of lineage holders and scholarly physicians. Imperial medical bureaus during China's dynastic periods systematized and preserved TCM knowledge, while rural barefoot doctors later adapted these principles for grassroots healthcare. This evolutionary process ensured TCM's relevance across social strata while maintaining its theoretical consistency.
Modern TCM education blends classical textual study with contemporary biomedical sciences, creating practitioners fluent in both traditions. The standardization of acupuncture point locations and herbal preparations facilitates global practice, while digital platforms now enable remote diagnosis using ancient assessment methods, demonstrating TCM's remarkable adaptability.
The Evolution of Design and Craftsmanship
TCM instrument development showcases millennia of medical innovation. Early acupuncture needles evolved from sharpened stones to exquisite gold and silver filigree, then to today's disposable stainless steel varieties. Herbal processing techniques like frying with honey or vinegar demonstrate sophisticated pharmaceutical knowledge predating modern chemistry. Contemporary research validates many traditional preparation methods, revealing how heating or combining herbs activates or stabilizes active compounds.
Social and Cultural Influences
TCM's development reflects China's philosophical and social history. Confucian values emphasize the physician's moral responsibility, while Daoist concepts shape diagnostic approaches. The integration of Buddhist medicinal knowledge during the Tang Dynasty enriched TCM's psychological dimensions, particularly in understanding mind-body interactions. Modern TCM retains these multidimensional perspectives while addressing contemporary health challenges like digital-age stress syndromes.
The Impact of Modernity on Style
Twenty-first century TCM synthesizes tradition with innovation. Electric acupuncture devices supplement manual techniques, while HPLC analysis ensures herbal quality control. Some practitioners incorporate functional medicine testing to quantify TCM pattern diagnoses, creating hybrid assessment models. This evolutionary process demonstrates TCM's living tradition status - firmly rooted in classical theory yet dynamically responding to modern healthcare needs.
TCM in the Modern World: Integrating Ancient Wisdom into Contemporary Healthcare

Traditional Chinese Medicine (TCM) and Modern Healthcare Systems
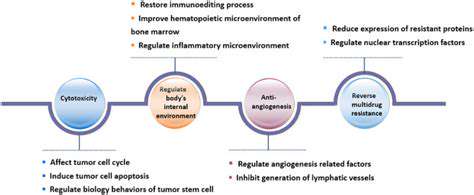
The dialogue between TCM and biomedicine represents one of contemporary healthcare's most promising frontiers. While Western medicine excels in acute care and surgical interventions, TCM's strength lies in managing complex chronic conditions through systemic regulation. Forward-thinking hospitals now develop integrated oncology programs where acupuncture manages chemotherapy side effects while herbs support immune function. This complementary approach maximizes therapeutic benefits while minimizing iatrogenic risks.
Acupuncture: A Deep Dive into the Technique
Modern neuroimaging studies reveal acupuncture's measurable effects on brain activity and pain perception pathways. The discovery of connective tissue planes corresponding to meridian lines provides anatomical correlates for ancient concepts. Clinical trials increasingly validate acupuncture's cost-effectiveness for conditions like chronic low back pain, prompting insurance coverage expansions in many countries.
Herbal Medicine: A Potent and Diverse System
Pharmacological research has identified active compounds in classic formulas like Gegen Qin Lian Tang for diabetes management. Advanced extraction methods now produce standardized herbal concentrates without losing the synergistic benefits of whole-herb combinations. Quality control innovations like DNA barcoding combat adulteration in the global herbal supply chain, ensuring patient safety.
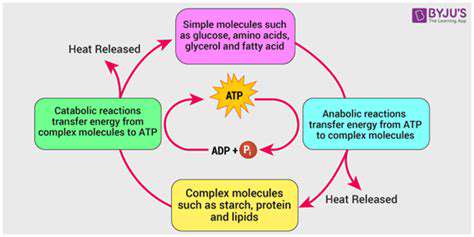
The Role of Diet and Lifestyle in TCM
TCM dietary therapy classifies foods by thermal nature and organ network affinities, offering personalized nutritional guidance. Contemporary research confirms many traditional observations, such as ginger's warming properties aiding digestion. Mind-body practices like Tai Chi demonstrate measurable benefits for balance, cardiovascular health, and stress reduction in numerous studies.
TCM and Chronic Pain Management
TCM's multidimensional approach to pain addresses both physiological and energetic aspects often overlooked in conventional treatment. Herbal anti-inflammatories like turmeric work synergistically with acupuncture's neuromodulatory effects. This comprehensive strategy reduces reliance on opioids while addressing pain's emotional and functional consequences.
Integrating TCM into Modern Healthcare
Pioneering integrative clinics develop protocols combining TCM diagnostics with Western testing, creating comprehensive treatment plans. Electronic health records now accommodate TCM pattern diagnoses alongside ICD codes, facilitating interprofessional communication. This integration requires respecting each system's strengths while developing shared treatment goals focused on patient-centered outcomes.
The Future of TCM in a Globalized World
As chronic lifestyle-related diseases increase worldwide, TCM's preventive and regulatory approaches gain relevance. International standardization of herbal quality and practitioner training ensures safe global practice. The next decades will likely see TCM concepts influencing mainstream medicine, particularly in systems biology and personalized treatment approaches.