TCM for PMS Symptoms: Balancing Your Cycle
Addressing PMS with Traditional Wisdom
The TCM Perspective on Menstrual Discomfort
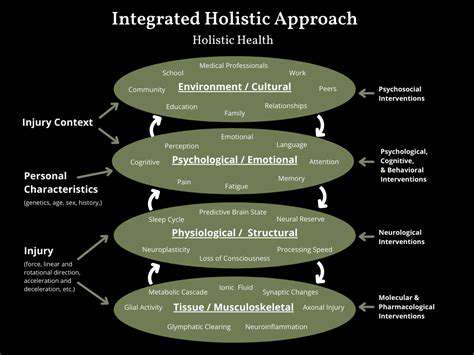
In Traditional Chinese Medicine philosophy, premenstrual symptoms reflect deeper energetic patterns rather than isolated issues. The dynamic balance between Yin and Yang energies becomes disrupted, creating various physical and emotional manifestations. What makes this approach unique is its recognition of how emotional states directly influence physical symptoms during the menstrual cycle. Rather than masking symptoms, practitioners seek to understand and correct the underlying energetic patterns creating the imbalance.
Energetic blockages often manifest as Qi stagnation or blood stasis, particularly affecting the liver and kidney meridians. These patterns aren't fixed - they evolve throughout the menstrual cycle and respond to lifestyle factors. Seasoned practitioners learn to read these shifting patterns to personalize their therapeutic approach.
Nutritional Strategies for Cycle Support
Diet plays a pivotal role in managing menstrual discomfort according to traditional principles. Certain food choices either support or disrupt energetic balance during sensitive phases of the cycle. Processed foods and refined sugars tend to aggravate symptoms, while nutrient-dense whole foods promote harmony. Warming spices like ginger demonstrate particular value, helping regulate internal temperature fluctuations associated with menstrual cycles.
Balancing Therapies
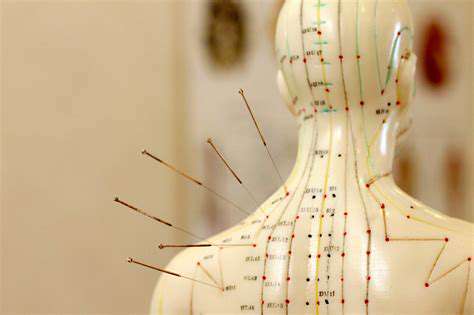
The strategic placement of fine needles at specific meridian points represents one of TCM's most recognized interventions. This practice aims to facilitate smoother energy movement, particularly in meridians relating to reproductive health. Clinical observations suggest these treatments may influence hormonal regulation through complex neuroendocrine mechanisms.
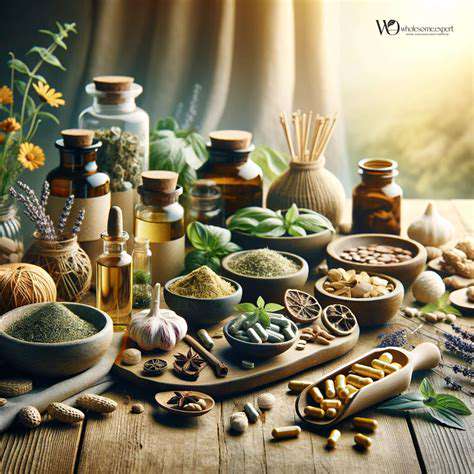
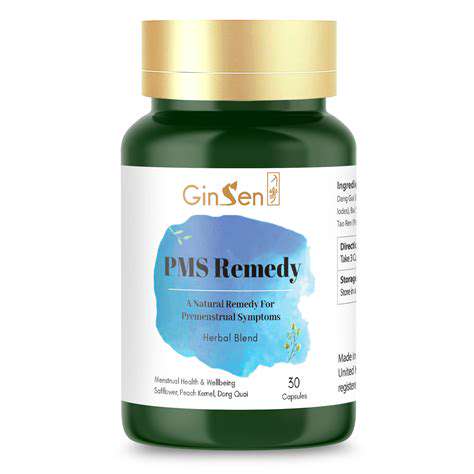
Herbal formulations represent another cornerstone of traditional practice. These botanical combinations address various aspects of menstrual discomfort - some focus on circulatory support while others target emotional aspects. Professional guidance remains essential as herb-drug interactions represent a serious consideration.
Supportive Lifestyle Practices
Beyond specific treatments, traditional wisdom emphasizes comprehensive lifestyle support. Movement practices like tai chi promote energy flow while mind-body techniques address emotional components. Sleep quality emerges as particularly crucial, as restorative rest supports the body's natural regulatory processes.
Stress management techniques take on special importance during the premenstrual phase. Breath awareness practices and meditation can help moderate emotional intensity naturally. These approaches encourage a more harmonious relationship with the body's natural rhythms over time.
Integrative Approaches to Menstrual Health
Needle Therapy Fundamentals
This ancient technique involves precise stimulation of anatomical points along energy pathways. Meridian theory suggests these points influence physiological processes through complex bioelectrical mechanisms. Modern research continues to explore how these interventions produce measurable physiological changes.
Clinical applications extend beyond pain management to include various functional disorders. The therapy appears to modulate nervous system activity while influencing endogenous pain modulation systems.
Plant-Based Support Strategies
Botanical medicine offers diverse preparations tailored to individual constitutional patterns. From traditional decoctions to modern extracts, these remedies address multiple aspects of wellbeing. The art of herbal formulation lies in creating synergistic combinations that address root causes while respecting individual variability.
Combined Modality Benefits
When integrated thoughtfully, needle therapy and botanicals often demonstrate enhanced effectiveness. This multimodal approach allows for addressing different aspects of imbalance simultaneously. Emerging research suggests combined protocols may influence inflammatory markers and hormonal regulation.
Therapeutic Considerations
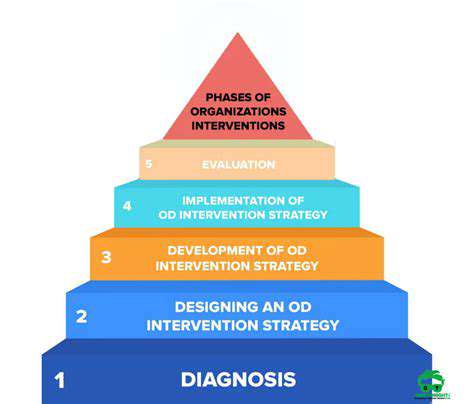
While generally safe when administered properly, these interventions require professional oversight. Practitioner selection remains paramount - look for extensive training and proper credentialing. Initial consultations should include thorough health histories and clear treatment plans.
Safety Protocols
Potential reactions vary from minor local responses to rare systemic effects. Transparent communication about all health conditions and medications ensures appropriate precautions. Ongoing monitoring allows for timely adjustments to treatment plans.
Selecting Practitioners
Quality of care depends heavily on practitioner expertise. Beyond basic credentials, seek professionals with specific experience in women's health concerns. Personal rapport and clear communication styles significantly influence therapeutic outcomes.